Well, after countless doctors’ opinions and a change of heart every half hour for a week, we’re back in Philadelphia for treatment. We opted for the intra-arterial chemotherapy from Dr. Shields. The procedure itself makes me very anxious, but in the end, this was best for our family for several reasons. It will hopefully kill the tumor in less than half the time, and will potentially cause fewer systemic side effects for Easton. He could lose his hair, he could be at risk for infection, but these aren’t guaranteed the way they would have been with systemic chemo. There are some scary risks during the procedure and to his eye afterward, but we know we’re in the care of competent doctors who are sought after by families all over the world for this treatment.

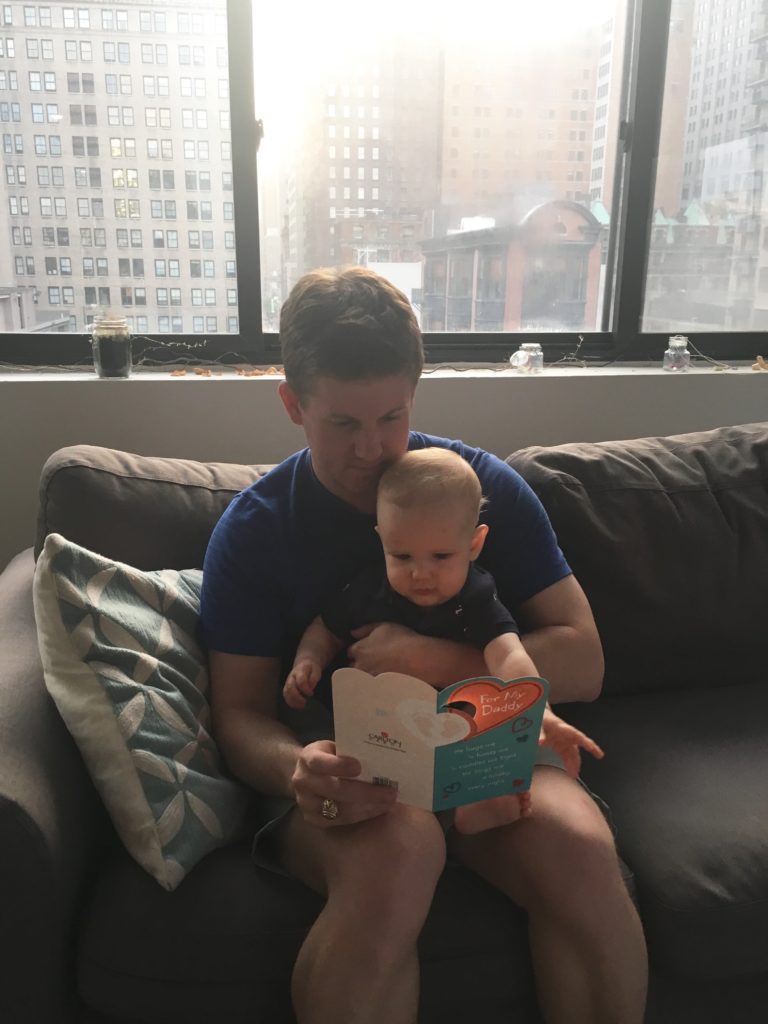
We were up all night before the flight out yesterday, still unsure of whether or not to come. Even when we got here and went to the doctor for pre-op, we didn’t know if we had made the right call. Our worst and weakest moment was last night. I was feeding Easton his bottle, and I just started bawling. He was looking up at me with those innocent eyes, studying my every move, every expression, taking cues for how he should feel and respond. It reminded me that this little life relies on us for absolutely everything, and in that moment, the weight of our decision crushed me. What if something terrible happens during the procedure? What if he wakes up blind, or worse? He is trusting us to keep him safe, and yet we chose the newer, more complex procedure with definite risks. Scott was ready to call and cancel, and I was ready to let him. There was so much guilt, so much fear. I prayed and prayed over him and tried to remind myself that there will be good and bad components of either treatment option. While we wholeheartedly trust that God is in control, we don’t always know exactly what that will like. We know that it may not be the vision WE have for our son and our family – this is where that little concept called faith comes into play. Once again, I fall short of what I’m called to do: I worry, I struggle with the unknown, I sometimes fear that God will use Easton for a purpose that doesn’t fall in line with my own selfish desires. THIS is where that little concept called grace comes into play. Thank goodness my doubts, fears, and selfishness have been forgiven before they ever even occurred. Thank goodness I have a Savior who has already paid the price for MY wrongdoing so that I may be worthy of a loving relationship with our Creator despite my shortcomings. It’s enough to bring peace over these worries and know that He deserves ALL the glory, no matter the outcome.

We checked in at Jefferson Hospital at 5:30am, and waited in pre-op until around 7:30am. We met with the anesthesiologist first, and then met the neurosurgeon, Dr. Jabbour. Dr. Shields controls the treatment call, which medicine and how much to use, and evaluates the tumor’s response, and Dr. Jabbour does the technical work of getting the medicine to the tumor. We knew how the procedure would work, but he took the time to draw out a picture of exactly what he was going to do and the alternate options he had if something didn’t go according to plan. He would insert a catheter into Easton’s femoral artery, then travel up through his aorta and carotid artery to the ophthalmic artery, which provides the blood supply to the eye. The medicine is given over a period of 30 minutes into this artery, then he pulls the catheter out. He does this procedure frequently, but it is quite complex. He explained the risks: small risk of stroke, small risk of blindness, risk that he would not be able to fit the microcatheter into the ophthalmic artery and be unable to perform the procedure, and risk that after this procedure, the artery shuts down and he is not able to perform this again. We won’t know if this happened until next month when the doctor goes in again and uses a dye to analyze the arteries before giving the second round of chemo.
I was able to walk Easton into the OR and be with him when he was put under. I hated leaving Scott alone; it was incredibly emotional and even the nurse was tearing up at our goodbye. After E was asleep, I gave him one last kiss and headed to the waiting area. The hospital was very good at keeping us informed. A nurse called my cell from the OR when they accessed his femoral artery and later when they accessed his ophthalmic artery, and Dr. Jabbour called when he was done to say everything went well. We were in the waiting room from 7:45-11:15, then met Easton in recovery. He had to be sedated for another 4 hours because he had to be still to prevent risk of bleeding. He woke up around 3:30, and after a little monitoring, we were released. We are monitoring his groin where the artery was accessed to make sure there is no bleeding, but aside from that, the directions are pretty simple. He’ll take half a baby aspirin each day for a week, but that’s about it. We’ll be scheduling his weekly blood work with our oncologist at home, and we’ll be back here in four weeks for another 5 days. For now, Easton is still pretty out of it, and we’ve had a very low key evening laying around in bed. We just have to stay in town for another 24 hours for monitoring, then we’re headed home!


 Thank you to everyone who sent prayers and good vibes our way. They were felt in a BIG way today!
Thank you to everyone who sent prayers and good vibes our way. They were felt in a BIG way today!